The 2026 Standards of Care in Diabetes, released by the American Diabetes Association (ADA), reflect a rapidly evolving diabetes care landscape – one that increasingly depends on nutrition expertise, individualized decision-making, and interdisciplinary collaboration.
For registered dietitian nutritionists (RDNs) and other nutrition professionals, the 2026 updates reinforce long-standing principles of medical nutrition therapy (MNT) while clarifying how nutrition care fits alongside expanding use of diabetes technology, obesity pharmacotherapy, and treatment of complex comorbidities such as chronic kidney disease, cardiovascular disease, and metabolic liver disease.
This overview highlights the most practice-relevant updates for nutrition professionals and what they mean for diabetes prevention and management.
Person-Centered, Inclusive Care Is Further Strengthened
The 2026 Standards continue the ADA’s emphasis on person-first, inclusive language and shared decision-making. Updated recommendations explicitly call for care plans that reflect an individual’s values, preferences, comorbidities, prognosis, and informed financial considerations.
For nutrition professionals, this reinforces the need to:
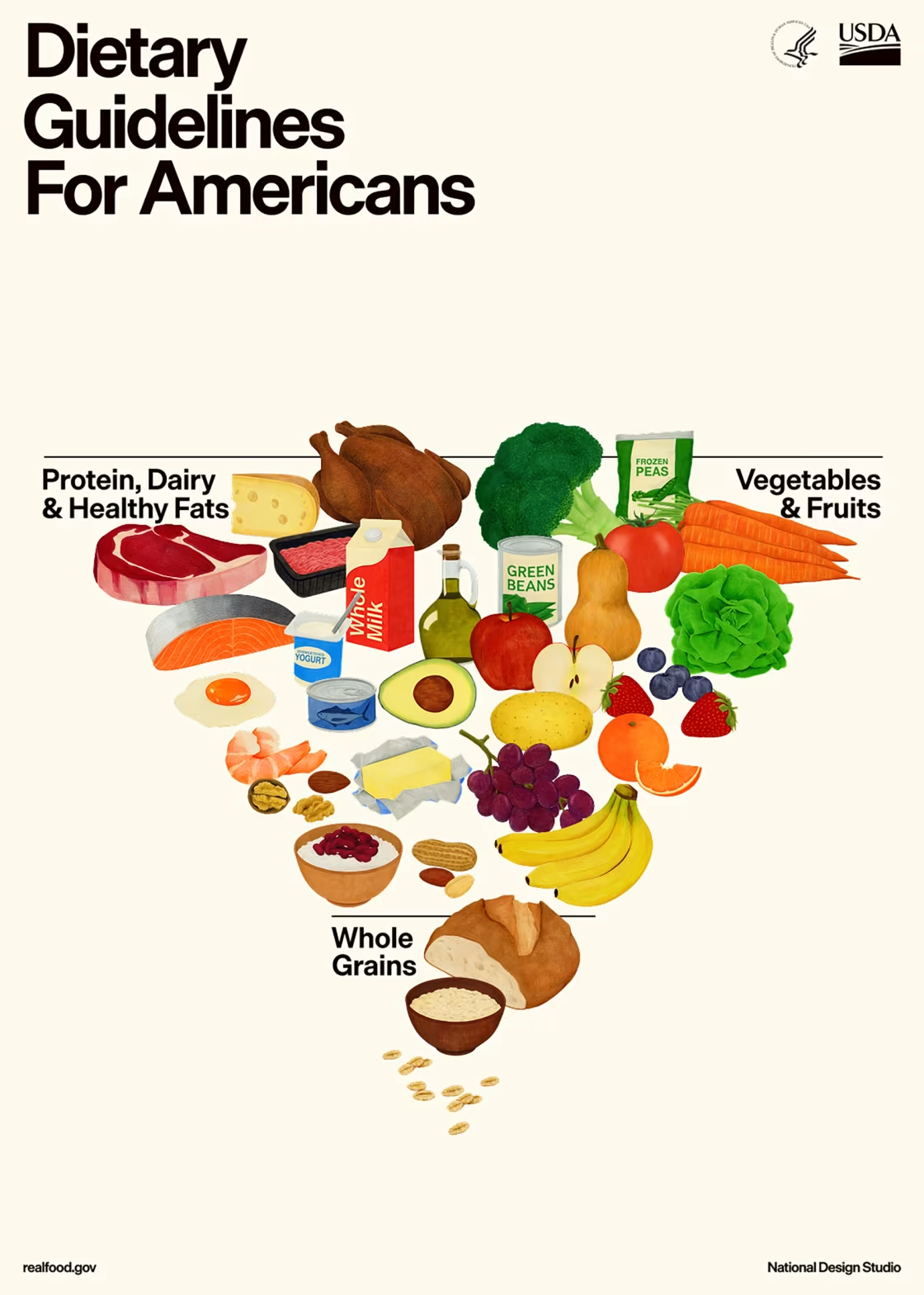
- Integrate cultural food practices and personal priorities into nutrition counseling
- Address affordability and food access as part of routine assessment
- Collaborate closely with care teams to align nutrition goals with medical treatment plans
Nutrition care is framed as an ongoing, individualized, and adaptive process, not a static set of dietary rules.
Diabetes Prevention: Clearer Nutrition Guidance and Broader Tools
The prevention or delay of diabetes section includes updates with direct implications for nutrition practice. The 2026 Standards clarify that eating patterns with the strongest evidence for preventing type 2 diabetes include Mediterranean-style and lower-carbohydrate eating patterns, moving further away from one-size-fits-all approaches.
Additional updates relevant to RDNs include:
- Continued emphasis on 5-7% weight loss for individuals with overweight or obesity at high risk
- Expanded use of telehealth, web-based, and smartphone-delivered diabetes prevention programs
- Consideration of continuous glucose monitoring (CGM) data when monitoring disease progression in select high-risk individuals
These changes highlight the expanding reach of nutrition-led prevention efforts, both in person and through digital platforms.
Medical Nutrition Therapy and Behavioral Support Remain Central
The 2026 Standards further strengthen the role of behavioral strategies within diabetes self-management education and support (DSMES). Nutrition interventions are closely linked with behavioral health, recognizing that sustainable dietary change requires more than education alone.
Key updates affecting nutrition practice include:
- DSMES should be culturally and socially appropriate and communicated across the care team
- Individuals pursuing intentional weight loss should receive regular monitoring for adequate nutrition intake
- Referral to behavioral health professionals is recommended when diabetes distress, anxiety, or fear of hypoglycemia is identified and warrants a higher level of care outside the scope of the nutrition professional
These recommendations underscore the essential role of RDNs in supporting long-term adherence, psychological well-being, and nutritional adequacy.
Weight Management and Obesity Treatment
Weight management remains a critical component of diabetes care, but the 2026 Standards place greater emphasis on individualization and safety. The guidelines reaffirm that modest weight loss improves glycemia and cardiometabolic risk, while also expanding guidance on pharmacologic and surgical options.
Notable updates include:
- Individualized dosing and titration of obesity pharmacotherapy to balance efficacy and tolerability
- Inclusion of obesity treatment options for people with type 1 diabetes, including GLP-1 receptor agonist-based therapies and metabolic surgery in select cases
- Ongoing nutrition monitoring to preserve lean body mass and prevent undernutrition
For nutrition professionals, these updates reinforce the importance of continuous nutrition assessment, especially as medical treatments become more complex.
Technology Expands and Nutrition Interpretation Is Essential
One of the most prominent updates highlighted in the ADA press release is the expanded role of CGM. The 2026 Standards recommend CGM at diabetes onset and anytime thereafter for individuals in whom it aids management, encouraging the removal of barriers to access.
While technology use increases, nutrition professionals play a critical role in:
- Interpreting glucose patterns in relation to meals and snacks
- Adjusting carbohydrate distribution, meal timing, and food choices using CGM data
- Helping individuals use glucose data constructively without increasing food fear or anxiety
As CGM and automated insulin delivery systems become more widely used, nutrition expertise is essential for translating data into meaningful action.
Chronic Kidney Disease, Cardiometabolic Risk, and Nutrition Care
The 2026 Standards include expanded guidance for people with diabetes and chronic kidney disease (CKD), including those on dialysis, as well as more detailed recommendations related to heart failure, metabolic liver disease, and cardiovascular risk reduction.
From a nutrition perspective, these updates highlight the need for:
- Careful coordination of nutrition therapy with evolving medication regimens
- Ongoing reassessment of protein, sodium, potassium, and overall nutrient intake as disease progresses
- Collaboration with interdisciplinary teams to balance glycemic control, kidney protection, and overall nutritional status
Nutrition professionals remain central to managing these overlapping conditions safely and effectively.
Special Populations: Nutrition Guidance Becomes More Specific
The 2026 updates provide more detailed nutrition-related guidance for several populations, including:
- Older adults, with specific recommendations for protein intake (0.8-1.5 g/kg/day or 15-20% of calories) and strategies to preserve lean mass
- Children and adolescents, emphasizing comprehensive nutrition education at diagnosis and annually, tailored to growth and development
- Pregnancy, with updated guidance on glycemic goals, CGM use, and medication transitions
These updates underscore the importance of life stage-specific nutrition expertise.
What This Means for Nutrition Professionals
The 2026 Standards of Care in Diabetes clearly position RDNs as essential contributors to:
- Diabetes prevention
- Individualized nutrition therapy
- Interpretation of glucose data
- Behavioral and lifestyle support
- Equitable, person-centered care
Staying current with these updates is critical for evidence-based practice and for confidently supporting increasingly complex diabetes care plans.
Go Deeper: 2026 Standards of Care in Diabetes Webinar
Understanding the Standards is only the first step. Applying them in real-world nutrition practice requires context, interpretation, and practical examples.
Our continuing education webinar is designed specifically for nutrition professionals:
2026 Standards of Care in Diabetes: From Guidelines to Practice
The webinar’s objectives are to:
- Explain the key revisions of the American Diabetes Association’s Standards of Medical Care in Diabetes, 2026.
- Integrate and individualize the current nutrition care guidelines when caring for adults with type 2 diabetes and related cardiometabolic conditions.
- Identify key times dietitians can assist clients with diabetes self-management education throughout the continuum of diabetes care.
- Recognize opportunities to facilitate relevant team-based care for the successful treatment and management of prediabetes and diabetes.
Learn more here:
https://www.beckydorner.com/product/2026-standards-of-care-in-diabetes/
Final Takeaway
The 2026 Standards of Care in Diabetes reinforce what nutrition professionals already know: effective diabetes care is individualized, ongoing, and grounded in nutrition expertise. As technology and pharmacologic options expand, the role of the RDN becomes even more critical, ensuring that care remains practical, patient-centered, and nutritionally sound.
High-quality continuing education helps bridge the gap between guidelines and practice, empowering nutrition professionals to deliver confident, evidence-based diabetes care.
Reference
American Diabetes Association Professional Practice Committee for Diabetes*; Introduction and Methodology: Standards of Care in Diabetes—2026. Diabetes Care 1 January 2026; 49 (Supplement_1): S1–S5. https://doi.org/10.2337/dc26-SINT













Connect With Us