Hypertension remains the most common and most modifiable risk factor for cardiovascular disease, chronic kidney disease, and cognitive decline. The American College of Cardiology and American Heart Association Joint Committee on Clinical Practice Guidelines recently published an updated guideline focused on the prevention, detection, evaluation, and management of high blood pressure in adults. This guideline replaces the 2017 version and introduces several important updates with direct relevance for registered dietitian nutritionists (RDNs).
For RDNs working in clinical, community, and population health settings, the 2025 guideline reinforces the central role of lifestyle and nutrition focused care, supported by stronger evidence and clearer clinical authority.
Hypertension Remains the Leading Modifiable Risk Factor
The guideline reinforces that high blood pressure is the most widespread and modifiable risk factor underlying cardiovascular disease and is strongly linked to coronary artery disease, heart failure, atrial fibrillation, stroke, dementia, chronic kidney disease, and all-cause mortality. Nearly half of adults in the United States meet criteria for hypertension, yet rates of awareness, treatment, and control remain far below national targets.
The recommended blood pressure goal remains less than 130/80 mm Hg for most adults. This emphasizes the importance of early intervention and sustained lifestyle support, rather than waiting until medication intensification becomes unavoidable.
Lifestyle Intervention Is Foundational, Not Optional
One of the strongest messages in the 2025 guideline is that lifestyle intervention is essential across the entire blood pressure continuum, from prevention to long term management of established hypertension. This is where RDNs play a critical role.
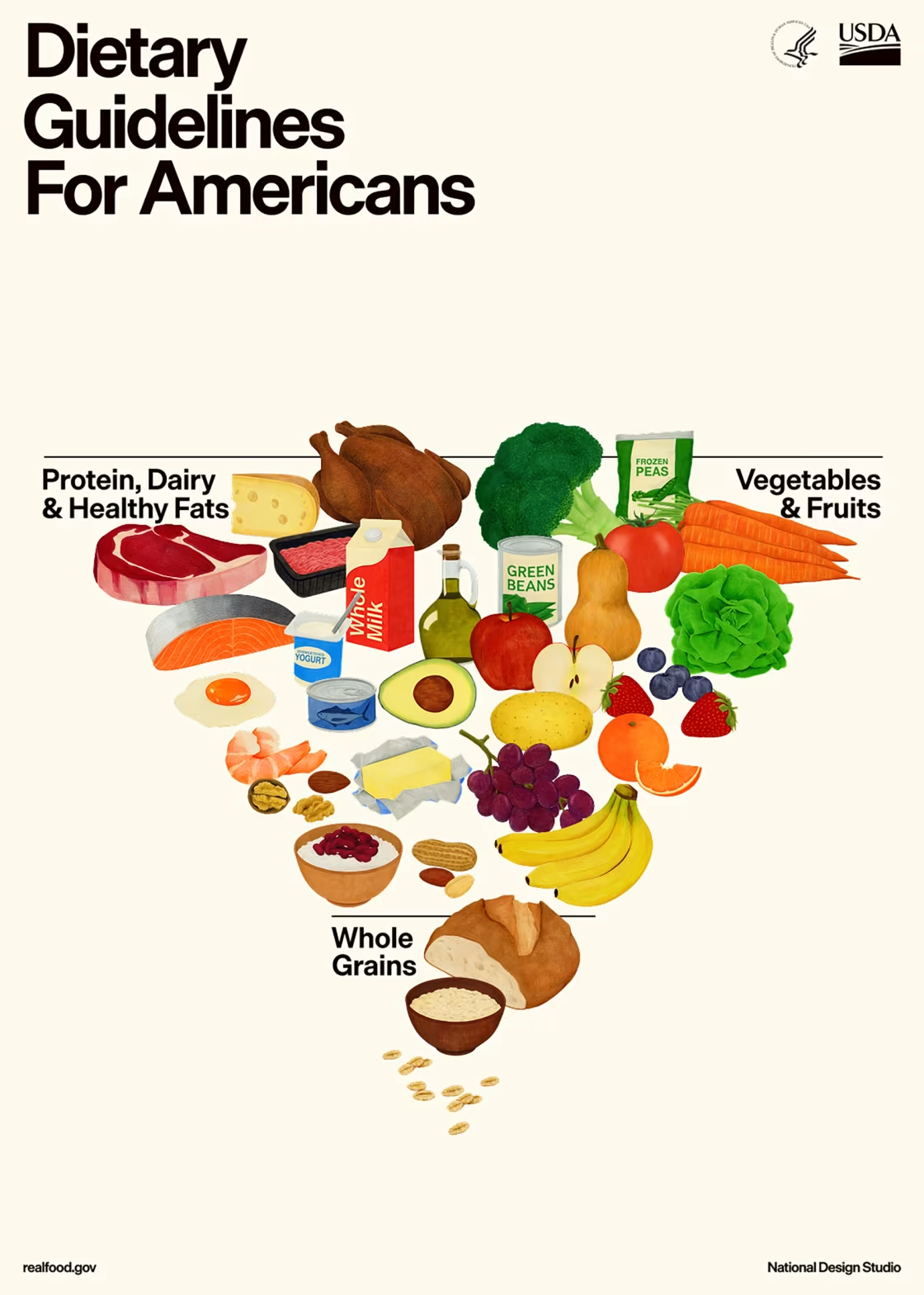
Key lifestyle recommendations include:
- Weight loss for adults with overweight or obesity
- Adoption of a DASH style eating pattern
- Sodium reduction to less than 2,300 milligrams per day, with an ideal target of less than 1,500 milligrams per day
- Adequate dietary potassium intake, primarily from food sources
- Regular aerobic and resistance physical activity
- Reduction or elimination of alcohol intake
- Stress management strategies
The guideline highlights that blood pressure tends to rise with age largely due to cumulative lifestyle exposures rather than aging itself. This reinforces nutrition intervention as a form of true primordial prevention.
New and Noteworthy for Nutrition Professionals
Potassium Based Salt Substitutes Are Supported
For the first time, the guideline explicitly supports the use of potassium based salt substitutes to help reduce blood pressure, particularly for individuals whose sodium intake is driven by home food preparation rather than packaged foods. This recommendation applies to adults without chronic kidney disease and without medications that impair potassium excretion.
For RDNs, this provides clinical support for practical flavor focused counseling strategies that go beyond simply telling patients to reduce salt.
Alcohol Guidance Is Clearer and More Direct
The guideline states that any alcohol intake raises systolic blood pressure in a dose dependent manner, even among individuals without hypertension. Adults who consume alcohol should be advised to pursue abstinence or limit intake to no more than one drink per day for women and two drinks per day for men.
This reinforces the importance of routine alcohol screening and counseling as part of nutrition assessment and intervention.
Risk Based Treatment Highlights the Value of Nutrition Care
The 2025 guideline introduces the PREVENT cardiovascular risk calculator, which estimates total cardiovascular disease risk and better reflects contemporary and diverse populations.
This shift has important implications for RDNs:
- More adults with mildly elevated blood pressure may qualify for early intervention
- Lifestyle therapy is emphasized as a first line approach before medication initiation in many cases
- Nutrition counseling during the first three to six months after diagnosis may determine whether medication is delayed or avoided
High quality nutrition intervention is positioned as a critical component of early risk reduction.
Home Blood Pressure Monitoring Supports Team Based Care
The guideline strongly endorses home blood pressure monitoring combined with multidisciplinary care to improve blood pressure control. Validated upper arm cuffs are recommended, while cuffless devices such as smartwatches are not recommended due to insufficient accuracy.
RDNs can support this process by:
- Reinforcing proper blood pressure measurement practices, including appropriate timing in relation to meals, caffeine intake, and physical activity.
- Helping patients interpret trends rather than isolated readings
- Connecting dietary changes to measurable blood pressure improvements to increase motivation
Health Equity and the Registered Dietitian Nutritionist’s Role
The guideline emphasizes team based care and recognizes the impact of social and structural factors on hypertension risk and control. RDNs are explicitly identified as essential members of hypertension care teams.
This strengthens the case for:
- Integration of RDNs into primary care and population health models
- Expanded access to medical nutrition therapy
- Community based nutrition interventions to prevent and manage hypertension
Key Takeaway for Registered Dietitian Nutritionists
The 2025 hypertension guideline places nutrition and lifestyle intervention at the center of blood pressure prevention and management.
It affirms that food patterns matter more than individual nutrients, early intervention changes long term outcomes, and RDNs are indispensable to effective hypertension care.
For RDNs, this guideline provides renewed clinical authority to do what evidence consistently supports: helping individuals eat and live in ways that support healthy blood pressure across the lifespan.
Call to Action
- Read the complete guidelines to review the full evidence base and detailed recommendations for hypertension prevention and management. To translate these guidelines into practical, client ready strategies, explore the Nutrition Guide for Counseling and Education, a comprehensive course designed to support effective nutrition counseling across clinical and community settings.
- Consider expanding your knowledge of nutrition education and counseling with one of these courses.
Reference
2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025;152:e114–e218. doi: 10.1161/CIR.0000000000001356













Connect With Us