The release of the new Dietary Guidelines for Americans (DGAs), 2025–2030, marks an important moment for nutrition professionals. As the foundation for federal nutrition policy, public health messaging, and many clinical and community-based nutrition programs, the DGAs significantly influence how nutrition guidance is translated into practice.
While many recommendations align with longstanding nutrition science (particularly the continued focus on nutrient-dense foods, reductions in added sugars, maintenance of saturated fat limits, and attention to fiber intake) other elements raise meaningful concerns related to clarity, consistency, and inclusivity. For registered dietitian nutritionists (RDNs) and other food and nutrition professionals, understanding both the strengths and limitations of the new guidance is essential for translating it responsibly into patient care, education, and policy advocacy.
Below, we outline key areas that align with scientific evidence, areas of concern, and implications for nutrition professionals in practice.
Areas of Alignment with Nutrition Science
Several components of the new DGAs reinforce principles that nutrition professionals have long supported and implemented in practice.
Emphasis on Nutrient-Dense Foods
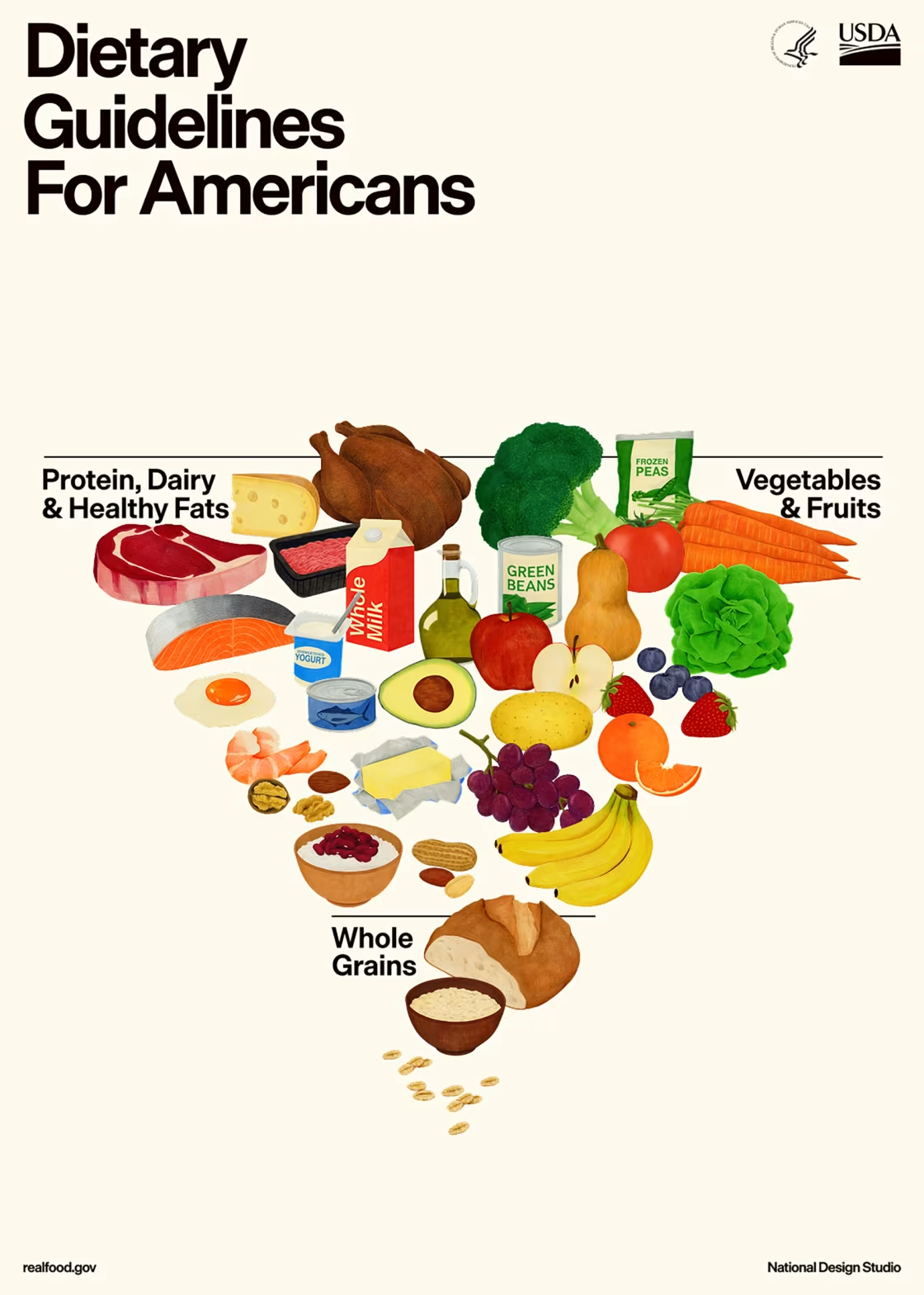
The continued prioritization of nutrient-dense foods including fruits, vegetables, whole grains, legumes, nuts, and seeds supports dietary patterns consistently associated with improved cardiometabolic health, micronutrient adequacy, and reduced chronic disease risk.
Limiting Highly Processed Foods and Added Sugars
Stronger language encouraging the reduction of ultra-processed foods and added sugars aligns with a robust and growing body of evidence linking these foods to obesity, type 2 diabetes, cardiovascular disease, and overall poor diet quality. This emphasis supports public health efforts to improve food environments and dietary patterns at the population level.
Retaining the Saturated Fat Limit
Maintaining the recommendation to limit saturated fat intake to no more than 10% of total calories remains consistent with decades of evidence demonstrating cardiovascular benefit when saturated fats are replaced with unsaturated fats.
Increased Attention to Fiber and Gut Health
Greater focus on dietary fiber and the role of the gut microbiome reflects emerging research connecting fiber-rich dietary patterns to improved metabolic, immune, and gastrointestinal health across the lifespan. This reinforces long-standing recommendations to emphasize plant-forward dietary patterns.
Areas of Concern
Despite these strengths, several aspects of the new DGAs raise concerns related to scientific consistency and real-world application.
Accessibility and Affordability Concerns
The new DGAs place increased emphasis on whole foods, including red meat and dairy, without sufficient consideration of affordability and access. For many individuals and families, these foods—particularly in higher-quality or minimally processed forms—are among the most expensive items in the grocery budget.
Cost remains a significant barrier to diet quality, especially for individuals relying on federal nutrition assistance programs or living in areas with limited food access. Recommendations that do not account for food cost variability and availability risk widening existing nutrition and health disparities.
Inconsistent Messaging Around Saturated Fat
The DGAs continue to recommend limiting saturated fat intake to less than 10% of total daily calories, a threshold supported by decades of evidence linking saturated fat reduction—particularly when replaced with unsaturated fats—to improved lipid profiles and reduced cardiovascular disease risk. This guidance is especially critical given that heart disease remains the leading cause of death in the United States.
However, this recommendation is difficult to reconcile with the increased emphasis on foods such as butter, beef tallow, red meat, and full-fat dairy. These foods are among the largest contributors to saturated fat intake in the U.S. diet, and even moderate portions can quickly push individuals beyond the recommended limit. Regular use of butter or beef tallow as primary cooking fats, frequent consumption of full-fat dairy products, or emphasis on red meat as a primary protein source can make it challenging to remain below the 10% saturated fat threshold—particularly within an individual’s caloric needs.
Substantial evidence continues to demonstrate that higher saturated fat intake, especially from animal sources, is associated with increased cardiovascular disease risk. Without clear guidance on portion size, frequency, and substitution with unsaturated fat sources (such as vegetable oils, nuts, seeds, and fatty fish), this messaging creates conflicting interpretations for both consumers and nutrition professionals.
For RDNs, this inconsistency complicates counseling and public health education efforts, as the promotion of these foods may inadvertently undermine adherence to the saturated fat limits the guidelines themselves continue to endorse.
Protein Quality and Source Recommendations are not Evidence-based
The DGAs significantly increase adult protein recommendations raising the recommended intake from the long-standing 0.8 g/kg of body weight per day to 1.2–1.6 g/kg of body weight per day. While this shift acknowledges the importance of adequate protein intake, particularly for preserving muscle mass and function with aging, the guidelines place limited emphasis on protein quality and source, focusing primarily on total intake.
Substantial evidence demonstrates that protein source matters. Diets higher in plant-based proteins (such as legumes, nuts, seeds, and soy) are associated with improved cardiometabolic outcomes and lower chronic disease risk, whereas higher intakes of red and processed meats are linked to increased risk of cardiovascular disease, type 2 diabetes, and mortality. Without clearer guidance on prioritizing protein sources, the increased protein targets may inadvertently reinforce dietary patterns higher in saturated fat and lower in fiber.
For nutrition professionals, this lack of nuance complicates counseling – particularly when balancing higher protein needs with cardiovascular health, kidney considerations, sustainability, and culturally diverse dietary patterns.
Alcohol Guidance is Ambiguous
Although the 2025–2030 DGAs adopt more cautious language around alcohol, the guidance remains insufficiently clear given the growing body of evidence showing that no level of alcohol intake is entirely risk-free. Even low levels of consumption have been associated with increased risk of cancer, cardiovascular events, and cognitive decline.
While the guidelines move away from suggesting health benefits of moderate drinking, they stop short of clearly promoting alcohol reduction or avoidance as a health-supportive choice. This ambiguity may perpetuate outdated perceptions about alcohol and health.
For RDNs and nutrition professionals, the absence of more definitive guidance increases the need to contextualize alcohol-related risks, address misconceptions, and translate evolving evidence into individualized, evidence-based recommendations.
Limited Consideration of Non-Dairy Dietary Patterns
The guidelines do not sufficiently address the needs of individuals who cannot or choose not to consume dairy, including those with lactose intolerance, milk protein allergy, those following cultural dietary patterns, ethical preferences, or plant-forward eating approaches.
This omission reduces the inclusivity of the guidance and overlooks the availability of well-established, nutrient-adequate non-dairy alternatives that can support calcium, vitamin D, and protein needs when appropriately selected.
Lack of Individualization for Various Populations
While the DGAs are intended for broad public health guidance, several recommendations lack sufficient nuance for diverse populations. Uniform messaging does not fully account for variation in health status, cultural dietary patterns, age, socioeconomic factors, or chronic disease risk.
Without clearer guidance on adaptation, the recommendations may be less applicable for populations such as individuals with food allergies or intolerances, culturally diverse communities, and those with limited access to food or healthcare.
Loss of a Practical Visual Framework
MyPlate served as a clear, effective visual teaching tool that helped translate the Dietary Guidelines into practical, real-world guidance. Its simplicity made the recommendations easier to understand and apply across clinical, community, and educational settings.
The absence of an equally accessible visual framework in the new DGAs may make the guidelines more difficult to operationalize, placing additional burden on nutrition professionals to translate complex recommendations for diverse audiences.
What This Means for Registered Dietitian Nutritionists and Nutrition Professionals
For RDNs and nutrition professionals, the new DGAs reinforce the critical role of professional judgment and individualized food and nutrition care.
Prioritize Dietary Patterns Over Individual Foods
Nutrition professionals should continue emphasizing overall dietary patterns rich in plant foods, fiber, and unsaturated fats, while also encouraging limited intake of ultra-processed foods. Rather than focusing on individual foods promoted in isolation, guidance should center on dietary patterns that prioritize minimally processed foods and appropriate preparation methods, which are consistently associated with improved cardiometabolic health, nutrient adequacy and reduced chronic disease risk.
Individualize Recommendations
The guidelines are not a substitute for individualized assessment. RDNs must continue to tailor recommendations based on the individual’s health status, chronic disease risk, cultural preferences, access, and personal values.
Clarify Conflicting Messages
As trusted nutrition experts, RDNs are uniquely positioned to help clients and communities navigate mixed messages—particularly around saturated fat, protein needs, and food sources—using the totality of the evidence.
Advocate for Inclusive, Evidence-Based Policy
The DGAs influence food and nutrition programs for all ages, food and nutrition reimbursement, and help set nutrition education standards. Nutrition professionals play an essential role in advocating for guidance that reflects scientific consensus, supports diverse dietary patterns, and prioritizes health equity.
Bottom Line
The new Dietary Guidelines for Americans include several positive, evidence-aligned recommendations that reinforce long-standing nutrition principles. However, inconsistencies in saturated fat messaging, limited inclusivity around dairy-free diets, ambiguous alcohol recommendations, and oversimplified protein guidance highlight the need for cautious interpretation.
For nutrition professionals, these guidelines underscore the importance of translating policy into practice thoughtfully—grounded in evidence, individualized care, and clinical judgement.
Reference
U.S. Department of Agriculture and U.S. Department of Health and Human Services (2025). Dietary Guidelines for Americans, 2025-2030. https://www.dietaryguidelines.gov/













Connect With Us