Becky Dorner & Associates exists to inspire excellence in nutrition care through in-depth continuing education programs, current industry information and helpful resources. The educational materials on this page are intended to help nutrition professionals expand their knowledge of the nutritional needs of individuals with chronic kidney disease.

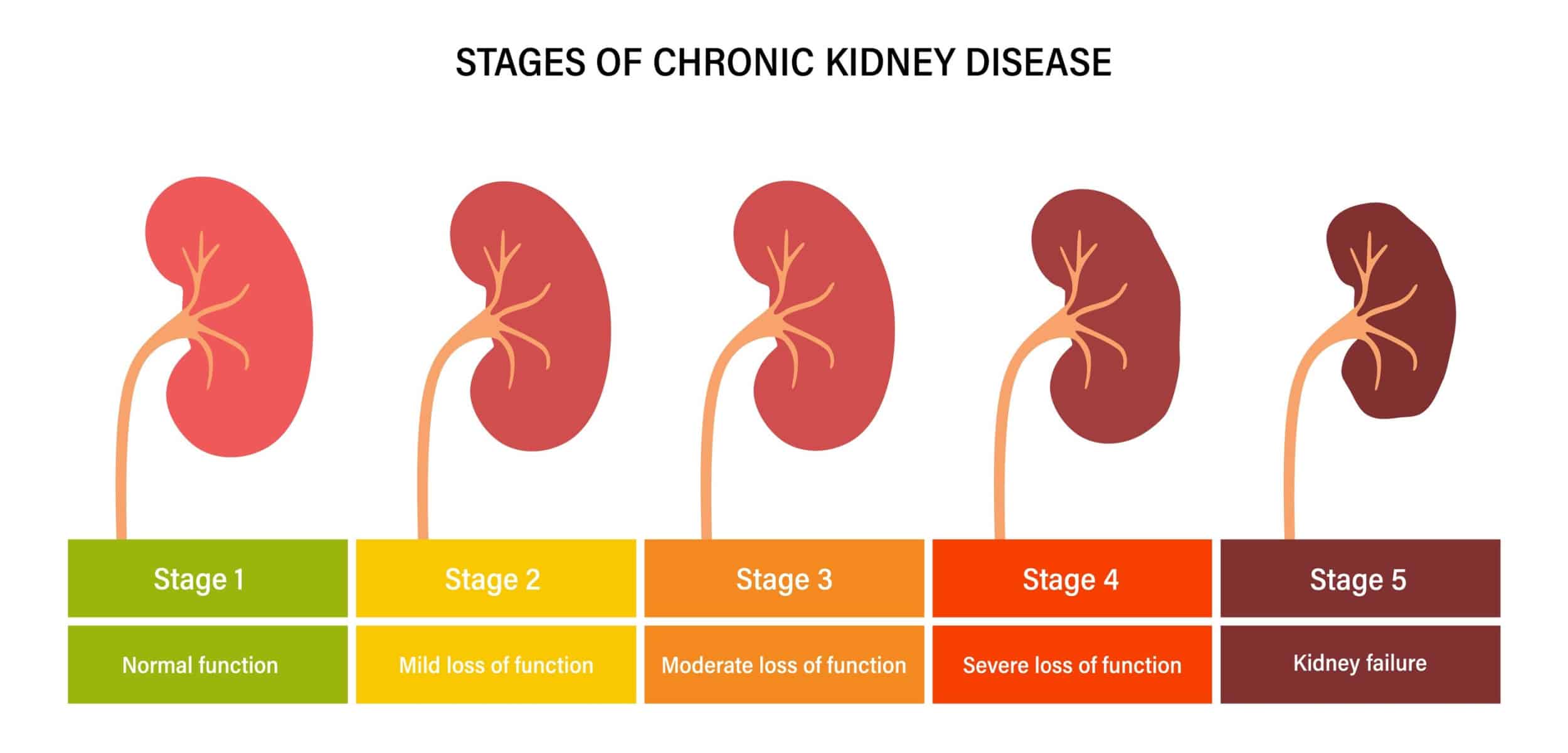
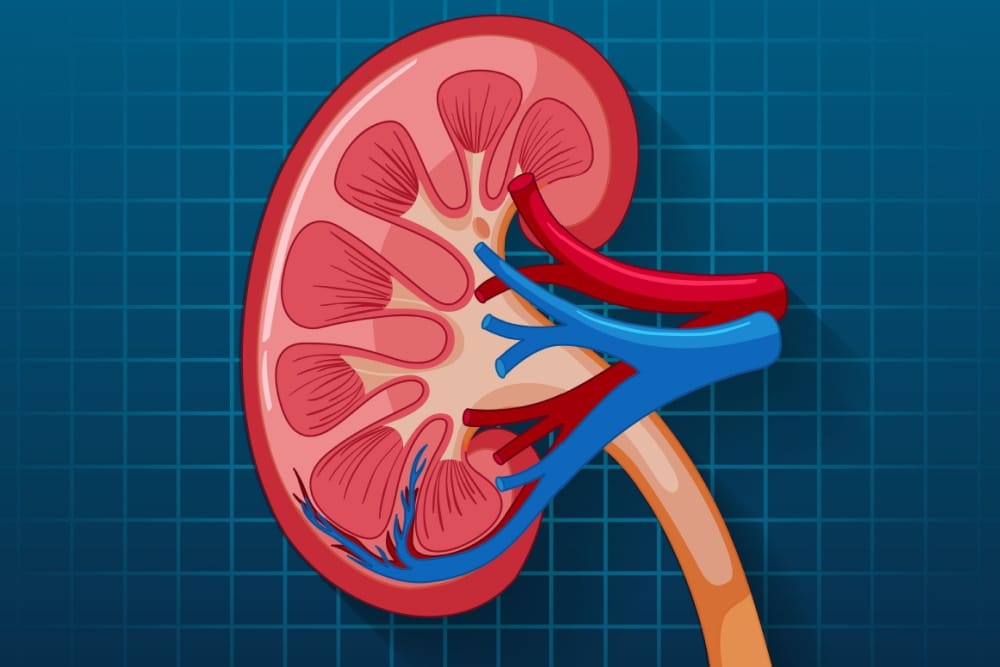
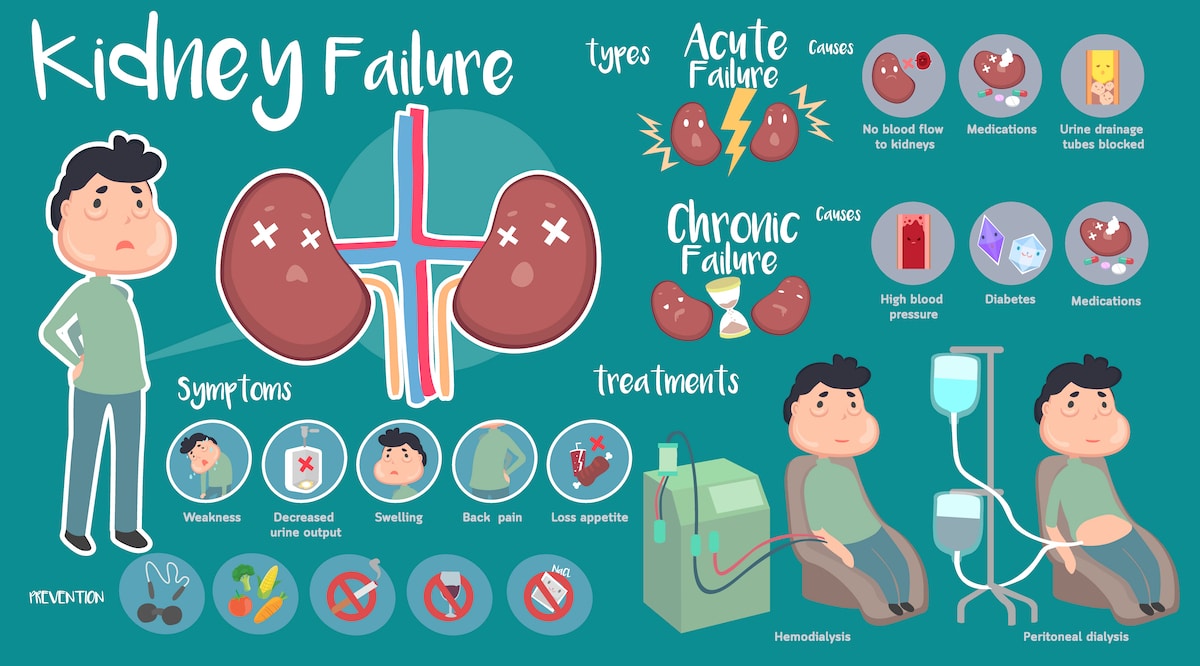
Chronic kidney disease (CKD) is a condition characterized by progressive decline in kidney function. When the kidneys are damaged, they are no longer able to properly filter blood in the body. Kidneys are responsible for getting rid of excess waste and fluid in the body, as well as the critical regulation of salt, potassium and acid content.1
The goal of treatment for CKD is to slow disease progression and prevent or slow related cardiovascular decline. The role of a nutrition professional in CKD treatment is to make customized nutrition recommendations based on the underlying conditions of the patient, including diabetes, hypertension, hyperparathyroidism, anemia and other conditions. In some cases, addressing the underlying etiology will slow or halt the loss of kidney function.2
Facts & Statistics Related to Chronic Kidney Disease
Let’s take a moment to understand the prevalence and causes of CKD:
- Roughly 11-13% of the global population is living with CKD.2
- CKD affects roughly 14% of adults in the U.S.3
- Diabetes and hypertension contribute to 70% of cases of CKD.2
- Roughly 30% of people with diabetes and 20% of people with hypertension develop CKD.3
- 90% of people who have CKD are not aware they have it.3
%
Population Living with CKD
%
Number of adults in the U.S. affected with CKD
%
Diabetes and hypertension contribution to CKD
%
Percentage of people who don't know they have it.
Sources
- National Kidney Foundation, How Your Kidneys Work. Updated 2023. Accessed June 29, 2023.
- PCRM’s Nutrition Guide for Clinicians, Chronic Kidney Disease. Updated February 3, 2023. Accessed June 29, 2023.
- National Institute of Diabetes and Digestive and Kidney Diseases, Kidney Disease Statistics for the United States. Updated September 2021. Accessed June 29, 2023.
CPE Courses on Chronic Kidney Disease
Webinars on Chronic Kidney Disease
Featured Blog Posts on Chronic Kidney Disease
MNT for Kidney Disease – What are the Best Resources for MNT?
If you ask any clinical dietitian what the most challenging subject is for patients to…Read More
Exploring Protein Energy Wasting in Chronic Kidney Disease
Protein Energy Wasting (or PEW) is an incredibly common issue for individuals who have been…Read More
Chronic Kidney Disease FAQs
Get answers to nutrition professionals’ most frequently asked questions about diet and nutrition care for individuals with chronic kidney disease below.
Please comment on low protein diets in the context of patients maintaining adequate muscle mass. Especially for seniors and those who exercise, I have read recommendations that protein intake should be much higher than the RDA for protein (1.2-1.5 gm/kg BW and/or 25-30 gms protein per meal). Can we safely have patients follow a low protein diet without adversely affecting muscle mass?
It is essential to understand what the goals are with an aging patient with chronic kidney disease (CKD), and working with the nephrologist will help to determine the direction of medical nutrition therapy (MNT). Low protein diets can place anyone at risk for malnutrition, so it is imperative that the composition of the diet assures that it meets energy and other nutrient needs. Monitoring outcomes and routine follow-up will be critical. Please also keep in mind that most evidence or recommendations for the general population do not apply to patients with CKD or end stage renal disease (ESRD) as this population is routinely excluded in study protocols.
Do you increase protein intake if patients are showing signs of protein energy wasting (PEW) yet still have CKD?
It is critical to prevent PEW in patients with CKD, so make certain that the patient is eating sufficient calories/energy and moderate the protein to replete or maintain an optimal nutritional status. Monitoring of dietary intake and patient outcomes are paramount in the earlier stages of CKD.
Why are patients with diabetes given more protein (0.8-0.9)?
Individuals with diabetes and CKD may be more prone to malnutrition, thus a bit more protein with special attention to ensure adequate calorie intake may be necessary to avoid this. Also, since proper management of diabetes is needed to slow progression of CKD, pulling too much protein out of the diet may jeopardize optimal glycemic control by subjecting individuals to too much carbohydrate. Allowing a bit more protein may be needed for a better balance of macronutrients to promote a more ideal glycemic control.
How do you balance the low protein requirements of a CKD patient with the increased requirements recommended for wound healing?
This is a very difficult clinical case. The best approach is to think about the most acute issue, which is the non-healing wound. It is critical to heal the wound, so you want to address the acute problem and not place the patient at further risk for protein-energy wasting or further health decline. Work with nephrology and attending physician to make sure CKD is managed through renal replacement therapies and prescribe a higher protein intake (along with other critical aspects of nutrient metabolism) to assure wound healing.
Any tips for RDNs that plan renal menus for long term care communities?
The application of the updated guidelines are appropriate for long term care populations as their needs are consistent with other CKD and ESRD patients. There is no evidence regarding any certain type of meal planning, so simply continue to use your best judgement. The Academy’s Renal Practice Group and Dietetics in Health Care Communities practice group have partnered on some resources or articles in the past and may be your best resources.
I see a lot of patients with reduced appetite while on HD that end up skipping meals - any tips for how to increase their food intake to make sure they meet their nutrition needs?
Unfortunately, the KDOQI guidelines do not cover recommendations for missed meals or nutrition supplements. Continue to monitor closely for changes in weight or protein status. Many patients remain remarkably stable despite missed meals due to reduced mobility or physical activity. Others may benefit from nutritional supplements, protein bars, protein cereals or more regular snacks. Review the options with patients and determine which may be best for them.
Is there a difference in fluid recommendations for HD vs PD patients or is it all based on urine output?
Yes, fluid requirements may be related to intake and output, as well as the hyperfiltration that occurs during the renal replacement therapies.
Does early restriction of potassium and phosphorus impact the speed of progression of CKD?
Unfortunately, with the large trial done three decades ago the Modifications in Diet and Renal Disease (MDRD) trial failed to show that restriction of phosphorus slows the progression of CKD. Additionally, none of the recent work examined supported that phosphorus restriction improves survival or mitigates progression. Phosphorus management needs to occur in order to prevent bone and mineral disorders which can indirectly lead to higher incidence of premature death. Potassium is not well studied but there is no evidence to suggest that dietary restriction will prevent kidney function declines.
If diet is adequate and labs look good except for high creatinine, what would be the recommendation for CKD stage 4?
There are certainly patients who have Stage 4 CKD with stable weight and normal range potassium and phosphorus levels. This is the scenario we would hope for in a patient who has had the expert guidance of a RDN, which is why it is so very important to educate providers regarding the need to refer those at risk of CKD to a RDN. The KDOQI nutrition guidelines would encourage you to continue with/encourage healthy dietary patterns such as the Mediterranean Diet and increased fruit and vegetable consumption to slow progression of CKD. Other important aspects would be a lower protein diet (goal 0.55 – 0.6 g/kg/day) with adequate calorie intake to maintain good nutritional status and a sodium intake <2.3 g/day for control of blood pressure/edema. Ongoing monitoring of the patient’s potassium level is key here as depending upon the types and amounts of foods consumed in these healthy dietary patterns, the diet can be quite high in potassium and it is in Stage 4 CKD that we can start to see a more dramatic drop off in potassium excretion via the kidney as well as an increase in acidosis, both of which can impact potassium balance, causing hyperkalemia.
For leaching potassium in potato, I have heard that you can boil them in a larger pot of water instead of soaking, has there been any research on that?
Yes, newer research on this subject has shown that soaking (aka leaching) is not an effective way to remove potassium from potatoes. Peeling and boiling, however, is very effective at removing potassium. The proper technique is as follows: 1) Peel potato and slice into thin slices or shred. 2) Put in pot with a large amount of water (10 times the volume of the potato). 3) Boil until tender. 4) Drain water and prepare as desired.
The following article shows that the peeling and boiling method removes 50% to 75% of the potassium. The greatest reduction of potassium occurs when the potatoes are shredded as there is more surface area available from which to remove potassium. Note this technique does not work for the Yukon Gold variety of potatoes. Reference: Bethke PC, Jansky SH. The effects of boiling and leaching on the content of potassium and other minerals in potatoes. J Food Sci. 2008;73(5):H80-85.
Disclaimer: The responses are for general information purposes only and are not intended to address individualized requirements. We have endeavored to keep the information accurate and refer the reader to resources that provide more detailed information, but this does not guarantee the accuracy of the Information. Becky Dorner & Associates accepts no responsibility, and no liability, for any loss or damage which may arise from using or relying on the information.
Free Resources on Chronic Kidney Disease and More
Blog
Check our blog regularly for new articles on popular nutrition care topics.

Email List
Subscribe to stay up-to-date on new products, sales, free resources and more

Free CPEs
Access free CPE courses and webinars to take your career to the next level.
The Essentials for Every Nutrition Professional
Browse Resources by Topic
Did you know you can now browse courses, webinars and other resources on our website by topic (in addition to Dysphagia)? We will be adding more topics soon!

Cardiovascular Health

Diabetes

Dysphagia

Malnutrition

Older Adult Nutrition
Request a Resource on Chronic Kidney Disease
Interested in learning more about older adult nutrition but don’t see the specific topic here? We’d love to get ideas for new resource creation. Submit the form below to tell us what we’re missing.
"*" indicates required fields