2021 Guideline for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: A Guideline from the American Heart Association and American Stroke Association
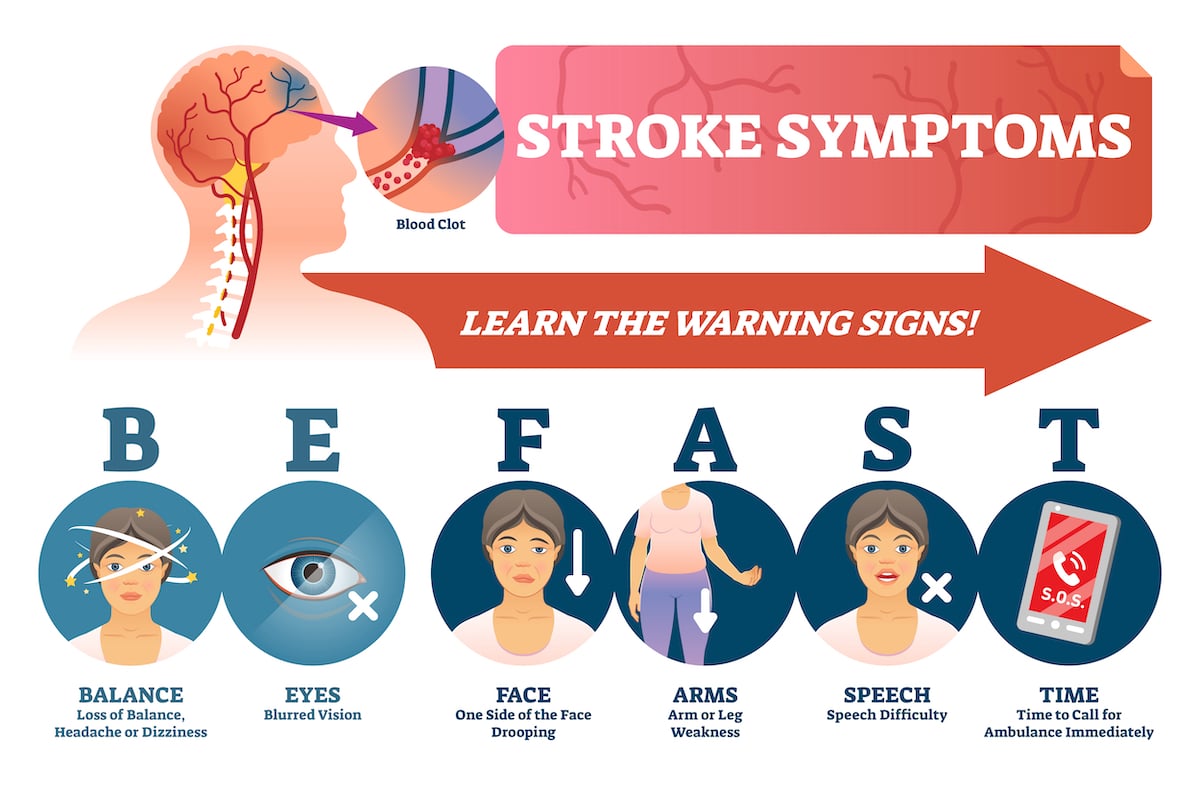
Nearly 800,000 people in the United States alone experience a stroke each year. Though most patients have a moderate risk of a secondary stroke, mitigation in most cases can be attainable through lifestyle modifications, diagnosis and treatment of contributing high-risk conditions and addressing health care inequities. Nutrition plays a role in controlling many of the lifestyle choices noted below.
Lifestyle Choices
First and foremost, reducing the risk of recurrent stroke rests mainly on the patient’s lifestyle choices, with the most significant contributing factors running the gamut:
- Blood pressure regulation
- Smoking
- Obesity
- Pre-existing hypertension
- Diabetes
- Sedentary lifestyle/physical activity
- Diet
In fact, one in three Americans is at risk in at least one of these areas. Evidence that supports lack of self-care as a high-risk contributor to recurrent stroke is overwhelming and unfortunate, but also highly encouraging, as lifestyle changes are challenging but attainable with training, a dynamic healthcare team, counseling, and a positive outlook.
While addressing and curtailing high-risk factors related to lifestyle and cerebrovascular disease, patients will likely require medical oversight and customized care.
Antithrombotic Therapy and Post-Stroke Care
Further, timely, thorough and individualized post-care treatment is essential. Antithrombotic drugs will likely be used in some form in nearly all cases without complications to lower bleeding risks and improved neurological results. After a stroke and on a case-by-case basis, patients will benefit from various anticoagulants, antiplatelet or other drugs. However, administering necessary therapies and maintaining quick, involved, and quality care often prove challenging.
Diagnosing and Treating High-Risk Conditions, Subtypes and Other Defects and Disease
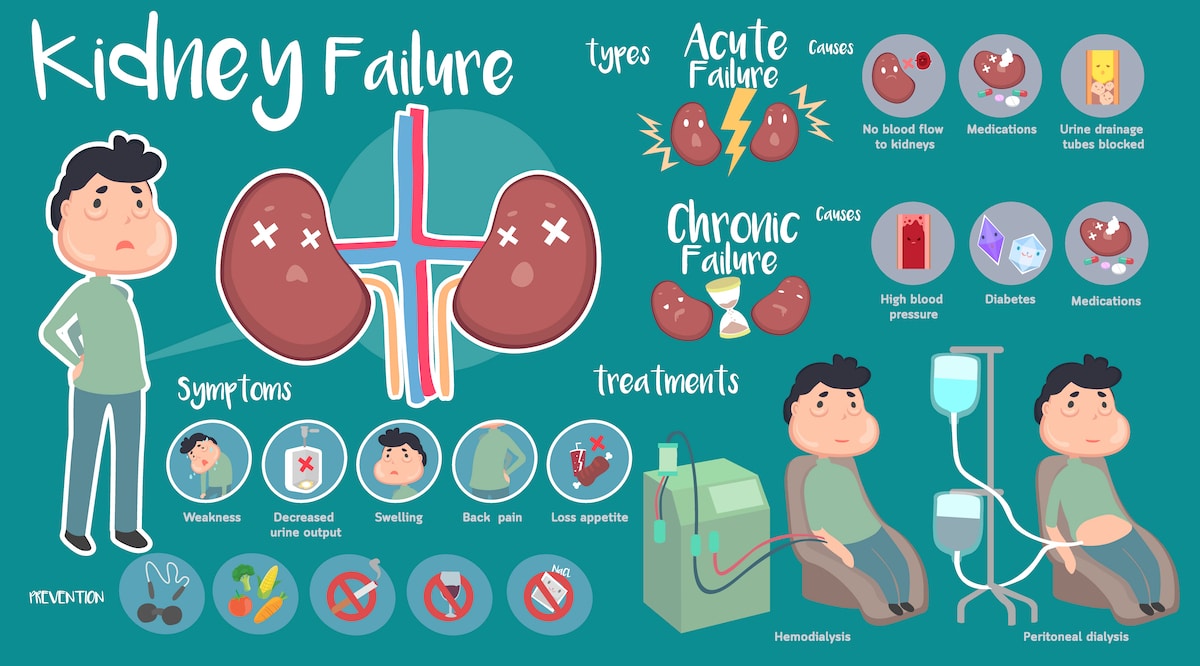
Conditions like atrial fibrillation, extracranial carotid artery disease, and intracranial stenosis are other common and treatable factors related to secondary stroke.
Additionally, dozens of other indicators like Anderson-Fabry disease, vertebrobasilar dolichoectasia, and fibromuscular dysplasia are more difficult to screen for and diagnose. In many cases, infectious diseases and even cancer may also influence risk.
Though all of these conditions are found and treated differently, each indicates a patient that has a high probability of recurrent stroke. Diagnosing and treating various underlying conditions is imperative to reducing the patient’s overall risk.
Race and Socioeconomic Status
Complicating things further, race, socioeconomic status, and sexual orientation are often contributing factors to recurrent stroke as well. People of color, women, the elderly, immigrants, residents of rural areas, and members of the LGBTQ+ community are less likely to receive thorough, guideline-recommended care. Standardizing care and addressing social inequities is complicated but key in addressing recurrent risk in specific demographics.
While the systematic methods and classifications for cerebrovascular health change year to year thanks to advancements in knowledge and technology, overarching ideas and guidelines should be utilized on a case-by-case basis keeping in mind the patient’s best interests, other health conditions, and quality of life.
Read the full article from the American Heart Association.












Connect With Us