Introduction
As part of the Affordable Care Act, the Centers for Medicare and Medicaid Services (CMS), highlighted the need for continuously improving the quality of patient care. One specific point of interest is an emphasis on reducing patient hospital readmission rates, with readmission being defined as “an admission to a subsection(d) hospital within 30 days of a discharge from the same or another subsection(d) hospital”.
The goal is to limit recurrent hospitalizations with a focus on six different conditions:
- Acute myocardial infarction
- Chronic pulmonary obstructive disease
- Heart failure
- Pneumonia
- Coronary artery bypass graft surgery
- Total knee or total hip arthroplasty. (1)
While physician care and medication regimens play a significant role in limiting hospital readmissions, experts suggest that malnutrition status and food insecurity are also key contributors. (2,3) Focused medical nutrition therapy (MNT) provided by the registered dietitian nutritionist (RDN) to address nutrition issues is essential to improve clinical outcomes and reduce hospital admissions.
Impact of Malnutrition
Malnutrition, particularly in the older adult, can negatively impact prognosis, mortality, hospital length of stay and readmission risk. (4) An estimated 20 to 50% of older patients meet the criteria for malnutrition before hospitalization. Malnutrition often worsens during a hospital stay because of inconsistent oral intake due to illness, medications, treatments, and other factors. (4) Despite available screening tools and malnutrition diagnostic criteria, routine evaluation and assessment for nutrition risk remains inconsistent with a lack of a universal method.(4) Establishing a protocol for early diagnosis and intervention can help improve identification of malnutrition and create a plan for nutrition intervention.
Screening and optimizing nutrition care for those identified with malnutrition can also have an impact on risk for hospital readmission. Multiple comorbidities, weakened immune function, increased frailty, lack of adherence to prescribed medication, and poor nutritional status can each contribute to this risk for the older adult. For individuals meeting criteria for malnutrition before or during hospitalization, risk is greater for readmission within 180 days. (3) To help offset this risk and as part of care provided by the RDN, nutrition intervention should focus on patient education, diet modification, and oral nutritional supplements as appropriate. In long term and post-acute care settings, if food intake is inadequate, goals may include diet liberalization with oral nutrition supplementation to support appetite and intake. (4)
Understanding Food Insecurity’s Impact
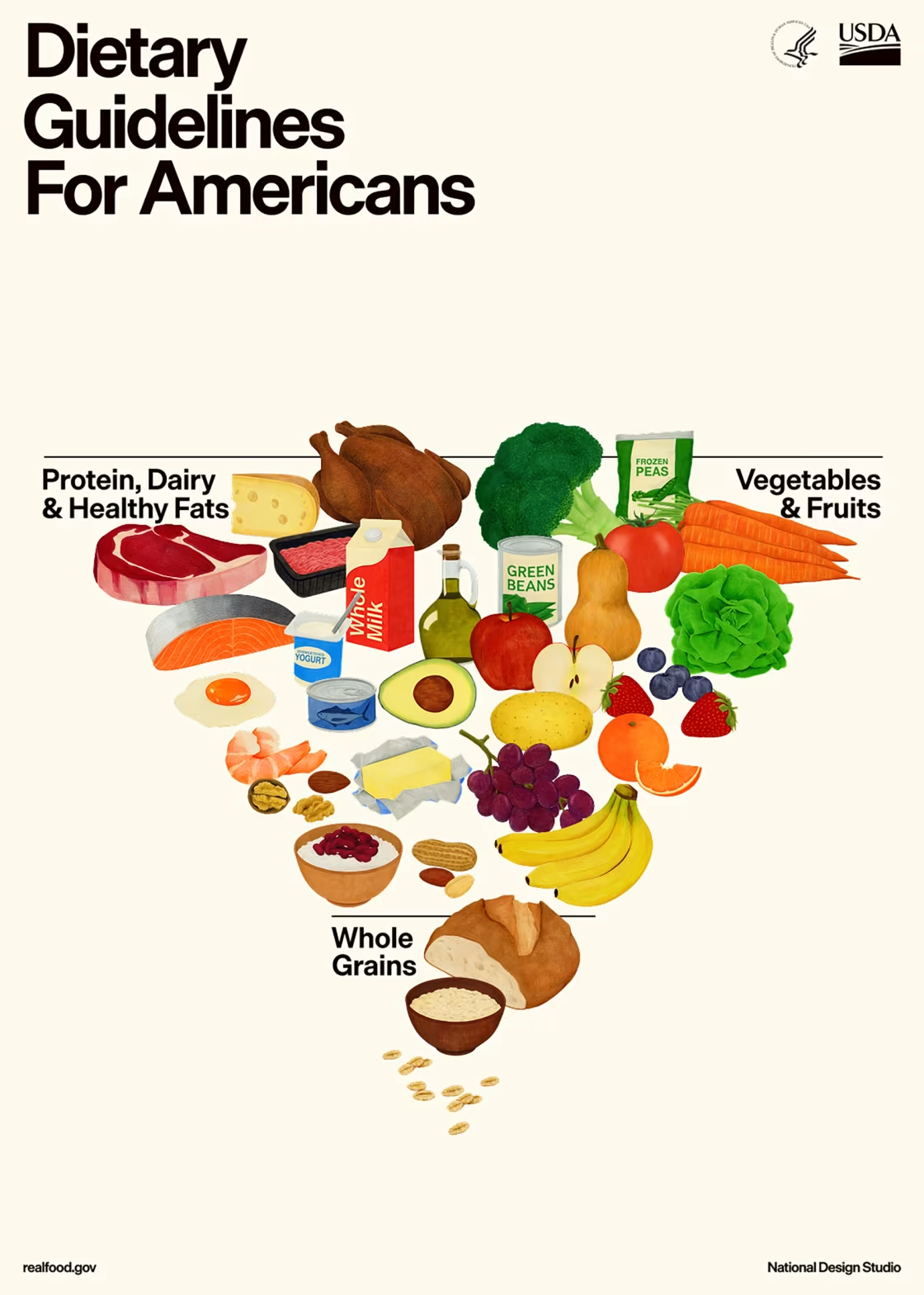
One out of eleven older adults are challenged by food insecurity. (5) Barriers to consistent food security may include fixed income as well as social isolation, chronic disease, increased medical costs, and unstable housing. Due to limitations in ability to prepare foods, food choices may be heavily processed and lacking in valuable vitamins and minerals. Insufficient funds may limit the ability to regularly purchase fruits, vegetables and other nutrient dense choices. (5,6)
Recognizing the impact of suboptimal nutrient intake on chronic disease, malnutrition and healthcare burden, experts focus on specific interventions for those at the highest risk. Programs are designed to support the individual’s health by encouraging use of community resources, patient education, medically tailored meals or groceries, and cost-effective options to allow for more consistent intake of fruits and vegetables. (6) Interventions to address food insecurity are essential for community dwelling older adults to limit the poor outcomes associated with frequent hospitalizations.
Call to Action
The RDN can play an essential role in enhancing patient care by identifying, care planning and intervening for those most at risk for malnutrition and food insecurity. With this in mind, the following steps can be implemented with the goal of helping to prevent hospital readmissions.
- Implement routine nutrition screening to identify malnutrition and/or food insecurity.
- Provide individualized nutrition education and resources for disease management to meet diet goals.
- Identify individualized, local community resources that may be of benefit to the patient.
- Care plan for home nutrition services after hospital discharge.
- Promote the importance of the role of the RDN within the intradisciplinary care team to improve overall patient care.
References
- American College of Emergency Physicians. Medicare’s Hospital Readmission Reduction Program FAQ.
https://www.acep.org/administration/reimbursement/reimbursement-faqs/hospital-readmissions-faq#:~:text=CMS%20(Centers%20for%20Medicare%20and,term%20inpatient%20acute%20care%20hospitals. Accessed November 22, 2024. - Swinburne M, Garfield K, Wasserman AR. Reducing hospital readmissions: Addressing the impact of food security and nutrition. J Law Med Ethics. 2017;45(S1):86-89. doi:10.1177/1073110517703333
- Iversen M, Buhl A, Schnieber A. Nutritional risk predicts readmission within 30 and 180 days after discharge among older adult patients across a broad spectrum of diagnoses. Clinical Nutrition ESPEN. 2023;61:288-298. doi: 10.1016/j.clnesp.2024.03.027
- Bellanti F, Burglio A, Quiete S, Vendemiale G. Malnutrition in hospitalized old patients: screening and diagnosis, clinical outcomes, and management. Nutrients. 2022;14:910. doi: 10.3390/nu14040910
- National Council on Aging. Aging in America: Get the Facts on Food Insecurity and Older Adults. https://www.ncoa.org/article/what-is-food-insecurity-get-the-facts/. Accessed December 2, 2024.
- Mozaffarian D, Aspry K, Garfield K, et al. “Food is Medicine” strategies for nutrition security and cardiometabolic health equity. J AM Coll Cardiol. 2024;83:843-864. doi:10.1016/j.jacc.2023.12.023
Also, search our courses and webinars and manuals for more on this subject.













Connect With Us